Professor Kiran Patel, Medical Director at University Hospitals Coventry & Warwickshire (UHCW) NHS Trust.
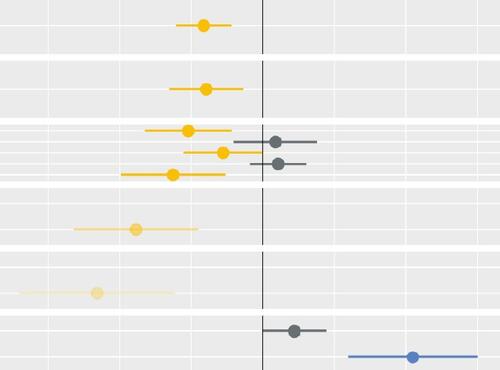
As the NHS emerged out of the pandemic, it was confronted with the challenge of not only recovery of unprecedented waiting lists, but with inequalities which required attention. NHS leaders challenged providers to restore inclusively and at University Hospitals Coventry and Warwickshire NHS Trust, we have developed a way of doing just that, whilst simultaneously reducing waiting times for all. Our team have built the Health Equity And Referral To Treatment tool (HEARTTTM) which uses clinical, social and demographic information alongside waiting times to prioritise patients based on needs. The next step with this tool is to include more information on patients’ status while waiting. There is no blue-print for this, quantitative analysis will only get us so far but will not answer the big questions - such as impact of waiting on mental health, employability, education or caring. Creation of an algorithm which takes into account individual need and potential outcomes will need a series of values-based judgements. This is a significant shift in thinking which can only be achieved in partnership with the public who will be affected.
The debate that we need to have with the public - what is important to them, what has greatest impact, what can, and should, the NHS take into account – is complex and can’t be explored or resolved through superficial engagement. Deliberative research offers the opportunity to engage in two-way meaningful discussion with time to delve into key questions and issues raised. By using this approach we have been able to develop the discussion based on what the public felt was important, for example recognising the steps that are needed to respond to the concern of some that explicit prioritisation methods might lead to some gamification. Partnering with Ipsos brought methodological expertise to the deliberative research approach. Importantly they also brought independence, they recruited participants from across our area enabling us to engage with a group that was wider than our usual patient engagement group and reflective of the local population. Ipsos ran the workshops, facilitated discussions and carried out the analysis, challenging our thinking and increasing the validity of the output.
We have an ongoing partnership with Midlands and Lancashire CSU Strategy Unit. They are exploring the issues and challenges of tackling health inequalities in the NHS and have published key quantitative and qualitative studies that are helping to shape policy. As well as funding and commissioning the deliberative research, members of the Strategy Unit team were part of the steering group and helped to shape the approach. They considered the results in the context of their related work, including both the legal and ethical aspects of health inequalities and prioritisation.
Most importantly in this work has been our partnership with the public. The 50-strong members of the group were really put through their paces, unpicking and discussing challenging topics across 12 hours of deliberation. This has resulted in several layers of information. On one level we have their views on what is important to consider when prioritising waiting lists – this is what we initially asked for. However the deliberation gave us so much more. The group identified and explored some of the challenges that we will face, such as data collection and achieving objective measurement proportionate to resources. There was also wider discussion about how far the role of the NHS should extend in tackling inequalities and what we can do better, such as “active waiting” and reducing DNAs.
So where next? The role of the NHS in tackling health inequalities will require ongoing engagement with the public and our patients. Individual risk factors that drive health inequality, such as disability and lifestyle factors, need to be considered alongside population-level factors such as ethnicity and deprivation. There are topics that need further exploration, in particular how the NHS can impact on wider determinants of health such as work, education and caring and how we apply social value judgements to these issues while avoiding unintended consequences. We need to apply this qualitative research within quantitative tools such as HEARTTTM. This is innovative work; we are not going to have all of the answers straight away but engagement through deliberative research with the public will guide and steer us along the journey.